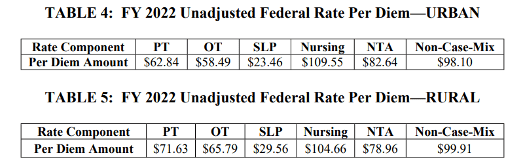
On April 8, 2021, the Centers for Medicare and Medicaid Services (CMS) released the FY 2022 SNF PPS Proposed Rule which will take effect October 1, 2021. As anticipated, changes to the Patient Driven Payment Model (PDPM) rates and Case Mix Indexes (CMI) are proposed. To begin, CMS proposes that the SNF PPS payment update is 1.3% as attributed to the market basket increase, forecast error correction, multifactor productivity adjustment, and in response to blood clotting factors indicated for the treatment of patients with hemophilia and other bleeding disorders (NTA and nursing services) being excluded from the Part A SNF PPS per diem payment. To provide for an appropriate proportional reduction in payments, CMS established a methodology for computing such offsets and proposes the updated, slightly higher rates seen below in Tables 4 and 5.
Unfortunately, higher base rates will not likely increase SNF reimbursement as CMS has included a proposed parity adjustment to better achieve the budget neutrality that was originally planned for the PDPM. Through data analysis, CMS has determined that there was a 5% increase in aggregate spending under PDPM for FY 2020, even absent the impact of COVID-19. To offset this increase, CMS intends to adjust the Case Mix Index (CMI) for each component of PDPM. How this will be achieved, however, remains to be seen as stakeholder comments are sought during the open comment period. The proposed rule includes a discussion of possible methodologies to recalibrate the PDPM parity adjustment via delayed implementation, a phased-in approach, or a combination of the two. Skilled nursing operators are being encouraged to start analyzing their operations in order to prepare for a possible reduction as industry leaders warn that SNFs could face a reduction of $12 per patient day if CMS does move ahead (McKnight’s, 2021).
CMS has also proposed several changes to the PDPM ICD-10 code mappings, some of which include:
- Sickle-cell disease, codes D57.42 and D57.44 will be assigned to “Return to Provider”
- Esophageal condition, codes K20.81, K20.91, and K21.01 will be assigned to “Medical Management”
- Multisystem inflammatory syndrome, code M35.81 will be assigned to “Medical Management”
- Vaping-related disorder, code U07.0 will be assigned to “Pulmonary”
- Anoxic brain damage, not elsewhere classified, code G93.1 will be assigned to “Acute Neurologic”
Additionally, CMS proposes to update requirements for the SNF QRP, including the proposal of two new quality measures beginning with the FY 2023 SNF QRP:
- SNF Healthcare Associated Infections (HAI) Requiring Hospitalization measure; and
- COVID-19 Vaccination Coverage among Healthcare Personnel (HCP) measure.
The proposed rule also outlines updates to the SNF Quality Reporting Program (QRP) and the SNF Value-Based Purchasing (VBP) Program, including a proposal to suppress the use of the SNF readmission measure for scoring and payment adjustment purposes in the FY 2022 SNF VBP program based on the determination that circumstances caused by the public health emergency for COVID-19 have significantly affected the validity and reliability of the measure and resulting performance scores.
To be considered, comments on this Proposed Rule must be received no later than June 7, 2021.
References:
- FY 2022 SNF PPS Proposed Rule https://www.federalregister.gov/public-inspection/2021-07556/medicare-program-prospective-payment-system-and-consolidated-billing-for-skilled-nursing-facilities
- Brown, D. (2021, April 13). SNF payments could drop by $12 per patient day under potential PDPM recalibration. McKnight’s Long-Term Care News. https://www.mcknights.com/news/snf-payments-could-drop-by-12-per-patient-day-under-potential-pdpm-recalibration/
Blog by Eleisha Wilkes, RN, RAC-CTA, RAC-CT, DNS-CT, Proactive Medical Review
Click here to learn more about Eleisha and the rest of the Proactive team.